Progressive Voice is a bi-weekly opinion column. The views expressed are solely the author’s.
Progressive Voice is a bi-weekly opinion column. The views expressed are solely the author’s.
By Patrick Hope
Virginia continues to make strides to reform our behavioral health system. Too many Virginians, some of them children and adolescents, lack access to basic preventive care and emergency intervention services. Many end up in our criminal justice system rather than being provided the necessary treatment to avoid such occurrences.
To address the gap, we in the General Assembly are laying a solid foundation on two fronts aimed at prevention–STEP-VA and Behavioral Health Redesign–with Gov. Ralph Northam’s proposed FY2021-22 budget making significant investments.
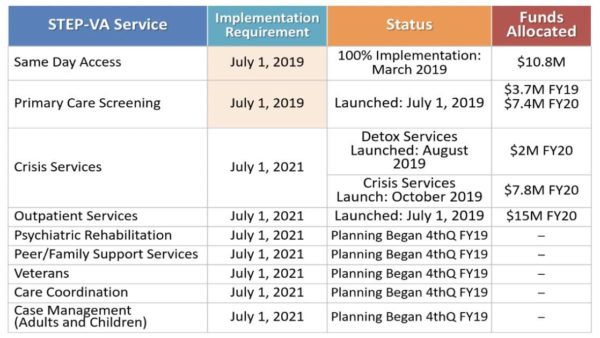
STEP-VA (System Transformation Excellence and Performance) was initiated to improve access, consistency, quality, and accountability of community-based behavioral health services.
- Same-day Access: The goal is to provide same-day access to a behavioral health assessment for anyone in crisis and to reduce wait times for services. We measure success when an individual can receive a follow-up appointment within 10 days from the initial assessment.
- Primary Care Screening: The goal in Phase 1 is to identify individuals who pose the greatest risk for physical health issues and connect them to primary care. Frequently, someone in crisis also has other health care issues: diabetes, heart disease, asthma, obesity. You have to treat the whole person and CSBs (Community Services Boards) have to connect the individual to primary care too. In Phase 2, we will expand primary care screenings to all consumers.
Since 2018, Virginia has appropriated over $60 million toward this effort, launching 2 of the 9 steps set for completion July 2021.
Behavioral Health Redesign seeks to integrate all behavioral health services to provide a continuum of care. The focus is on access to services that are: high quality regardless of the setting (e.g., home, school, and primary care); evidence-based (e.g., preventive care and care provided in a least restrictive environment); trauma-informed to yield better outcomes; and cost effective.
The goal with Redesign is to provide alternatives to involuntary hospitalization (Temporary Detention Orders or TDOs) and lower our reliance on inpatient psychiatric beds. Virginia still lacks alternatives to crisis services, such as outpatient treatment, leading to a significant increase in the number of court-ordered TDOs. My legislative efforts in the 2020 session will be to make reforms so that we can provide more appropriate care in a least restrictive environment.
Solving Virginia’s Psychiatric Bed Shortage
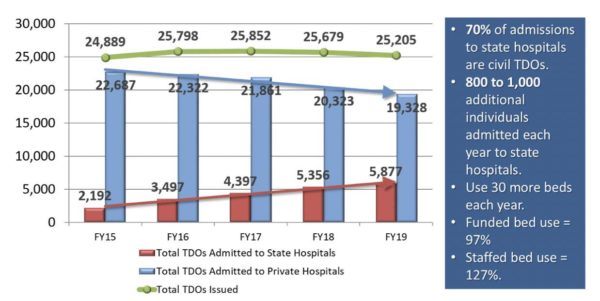
While the goals of STEP-VA and Behavioral Health Redesign are preventive, they have not had the full impact and Virginia continues to face a shortage of psychiatric beds. State hospitals have seen the number of TDOs more than double since FY2015, while private hospital TDO admissions have decreased (Figure 2). At the same time, according to the Virginia Hospital and Healthcare Association, private hospitals have seen an increase in voluntary admissions from 25,526 in 2015 to 29,278 in 2018, an increase of almost 15 percent.
Statewide TDOs and Hospital Admission Trends
TDO admissions in state hospitals have been rising, and those hospitals are operating above capacity. As of September 2019, state hospitals were operating at 101% capacity.
So solving Virginia’s psychiatric bed shortage will garner a great deal of attention this session with the debate on how best to do it. Gov. Northam proposes to add 56 new beds at Catawba Hospital, just outside Roanoke, at an annual cost of $10 million. He also proposes to add $16 million annually to encourage private hospitals to accept more TDOs.
Generally, I believe resources are better spent investing in community-based services rather than inpatient psychiatric beds. And that is the national trend — away from inpatient hospital spending (22%) and more toward community mental health spending (75%).
In Virginia, however, community mental health and inpatient hospital spending are roughly equal. In the long-term, investing more resources into psychiatric beds is going in the wrong direction but may prove to be necessary in the short-term, temporarily.
Behavioral health reform remains one of Virginia’s highest priorities. While it is sometimes not as “visible” as a physical ailment or disease, behavioral health painfully affects the lives of thousands of individuals and their families. And postponing or reducing effective treatment just makes the situation worse over time. That’s why I am so committed to funding the changes we need to strengthen behavioral health in Virginia.
Patrick Hope is a Delegate from the 47th District representing Arlington County. He is a member of the Joint Subcommittee to Study Mental Health Services in the Commonwealth in the 21st Century.