
More than 150 weeks have passed since Dr. Mike Silverman, the emergency department chair at VHC Health, started his Friday night posts about the Covid pandemic.
The public Facebook posts have helped provide medical context and clarity, but in layman’s terms, to those seeking a better understanding of the disease and the response to it. ARLnow has regularly quoted Silverman’s posts in our coronavirus coverage.
Now, three years after Silverman’s first pandemic post from the ER, he’s wrapping up the weekly series. While not ruling out occasional updates, Silverman says now seems like a good time to conclude his Friday writing routine. By Silverman’s count, he has produced more than 195,000 words of updates on the local prevalence of Covid, as seen at the hospital, and the latest medical research on the virus and its treatments.
“Stopping on the second Friday in March three years later seems like a good run,” he wrote last month when announcing the decision.
When Silverman published his first Facebook update on March 13, 2020, only five Arlington cases had been confirmed, local grocery stores were being picked clean and Arlington Public Schools had just announced the closure of schools through spring break in April. The first confirmed case in the county had been announced just four days earlier.
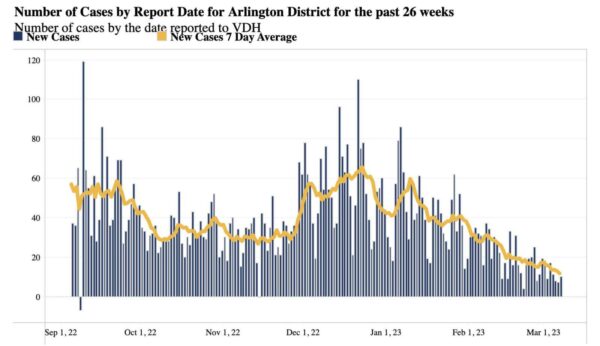
Today, with vaccines and three years of exposure to the virus, it is still deadly and debilitating for some, but not nearly to the extent of earlier, when it was still a novel outbreak. As of last week, cases in Arlington were down to an average of just 11 per day, the lowest point since mid-2021, according to Virginia Dept. of Health data.
The last confirmed Covid-related death in Arlington was reported during the final week of 2022.
“Coronavirus is not quite done with us yet though we’ve learned to live with it,” Silverman wrote on Friday.
That last weekly post is reprinted below with his permission.
It’s been another good week when it comes to the number of COVID cases we’re diagnosing in the ER. Our symptomatic positives are way down, with only a handful of positive cases and a 3% positivity rate this past week (6 week running average 10.3%). This is the second week in a row that is notably less than the previous weeks. Our general screening population (in theory asymptomatic patients or those we think COVID is unlikely) is also below 4% for the second week in a row (6 week average about 6%). The numbers for all comers this week show a 3.7% positivity rate and the last two weeks each had about half the number of cases we saw in the weeks beforehand. These numbers are consistent with other periods of time after surges. The number of hospitalized patients with COVID also dropped about 20% since last week. Hospitalizations climb in the weeks following a surge and are a lagging indicator of when the surge is over. I suspect we’ll continue to see a drop in the number of patients hospitalized with COVID over the next few weeks as well. However, I do anticipate that taking care of COVID patients in the ER and in the hospital will be part of our world for a long time to come.
I don’t think we really understand the long-term consequences of COVID yet. After all, if we were just learning about chicken pox, it would take years, potentially 20-40, to put it together with Shingles. Scientists are learning about Long COVID, but we have a way to go. About 10% of people are impacted by Long COVID. In a pre-print study out of The Lancet earlier this week, scientists looked at the impact of metformin, ivermectin, and fluvoxamine on the impact of reducing Long COVID. This was a well-designed, randomized, placebo-controlled study with 1125 patients who completed 9 months of follow up. The incidence of Long COVID in the placebo group was 10.6% and this was similar to ivermectin and fluvoxamine. However, the metformin group had a 6.3% incidence, which is a 42% relative reduction in incidence. Metformin is used for diabetes and patients had to have a BMI >30 and the medications were started within 4 days of symptom onset. I don’t see us adding metformin to the treatment cocktail for patients diagnosed with COVID, but I believe this will help scientists better understand future treatments for Long COVID.
We know that COVID can impact pretty much all our organs. In a study out of the VA, it looks like patients who had COVID were 36% more likely to have GI problems (most commonly acid disorders) than patients who did not have COVID. The VA database has 5.6 million patients and this study compared records of 154K patients.
This next study may not surprise you. Through the years, before COVID, I’ve certainly sent my kids to school when they were a “little sick.” I also took care of many COVID patients who had no intention of staying home from work and quarantining (which is very unfortunate and ultimately led to spread of disease). Now, a study published earlier this week in JAMA Open Network: “Some parents in the United States were dishonest about their children having the coronavirus or did not follow testing and quarantine guidelines, according to a study” that also found “some parents were dishonest about their children’s vaccination status.” For this study, “researchers analyzed answers by 580 parents who had children under the age of 18 living with them during the course of the pandemic.”
So here we are, as I’m trying to wrap up the weekly Friday Night Update posts. My first post was March 13, 2020. Since then, we’ve had 156 weeks or 1096 days. My word document is about 195,000 words and 333 pages.
I’ve had some conversations with non-medical friends this week about the beginning of the pandemic. It’s almost hard to remember how bad it was. I get the Facebook memories of my posts that pop up. I don’t always re-read them, but I have read some from the early months and it’s truly amazing how far we’ve come. Though, I don’t think we should forget how bad the pandemic was prior to the vaccine and how many people died. Over 1.1 million Americans have died of COVID and we’re still seeing about 1800 deaths a week.
I want to thank everyone for all the support you’ve given me with these pieces. It’s been incredibly helpful to me and helped me get through the worst of the pandemic. I’ve loved connecting with patients and readers and sharing my view of COVID as an ER doc with you. I appreciate the requests to post monthly or quarterly. I imagine I’ll continue to post as things happen but will enjoy the flexibility to do it on my schedule. If I see spikes in the COVID data, I’ll let you know. I’ll also try to post on other key treatment issues and other hot topics from the ER. If you have questions or topics you think would be interesting to other readers, send me a message. Some of the best posts have been in response to questions from readers.
If you’re wondering what I’m going to do with my Fridays, I am hoping to take the time I spend on these posts and put it towards something else, which will also include my real job and other writing obligations I have. For those interested, I could see using these posts to tell our story in a book with some additional behind the scenes info that I didn’t put on Facebook at the time. I’ll keep you posted. Thank you again for all your support and positive feedback. Working through the pandemic has been the most challenging and rewarding part of my career. These posts have contributed to that, and I can’t thank you, the readers, enough for that.
Coronavirus is not quite done with us yet though we’ve learned to live with it.
Science matters. Get vaccinated (or your booster)–the data clearly shows vaccines have saved lives. Keep a mask handy, even if you’re not routinely wearing them.
Mike

